Neuropsychopharmacology: Brain and Cardiovascular Responses to Acute Stress in Remitted and Recurrent Late-Life Depression
Among older adults who successfully achieve clinical remission from depression, 35%-45% will experience a new depressive episode within two years. The factors that contribute to the emergence of recurrent depressive episodes in older adults are not well understood. Psychological stress may play a role in depression remission and recurrence, yet important questions remain about the brain and physiological profiles of older adults with remitted depression, and the role stress pathways may play in depression recurrence in these patients.
Investigators including Thomas Kraynak, PhD (Assistant Professor of Psychiatry); Helmet Karim, PhD (Assistant Professor of Psychiatry and Bioengineering); Layla Banihashemi, PhD (Associate Professor of Psychiatry and Bioengineering); Meryl Butters, PhD (Professor of Psychiatry and Clinical and Translational Science); and Carmen Andreescu, MD (Professor of Psychiatry), from Pitt Psychiatry, examined how subjective, physiological, and brain responses to a psychological stressor differs in older adults with and without remitted depression, and how these stress responses relate to future relapse.
“We know that stress plays a major role in depression. Adults with depression tend to show altered brain and physiological responses to psychological stress. But it is less clear if these altered responses continue to manifest when depressed older adults are successfully treated and achieve clinical remission.” said Dr. Kraynak, first author of the current study, published in Neuropsychopharmacology. “Importantly, we also do not know if patterns of stress responses commonly observed in late-life depression also confer additional risk for a future, recurrent depressive episode.”
The investigators studied 76 individuals over age 60 who had recently achieved clinical remission from depression, as well as a comparison group of 36 age-matched adults with no history of depression. Participants completed an acute psychological stressor task during functional brain imaging with behavioral and cardiovascular monitoring. Participants with remitted late-life depression were followed longitudinally for up to two years to evaluate depression recurrence. The study was conducted across three sites and included colleagues at University of Illinois-Chicago and Vanderbilt University Medical Center.
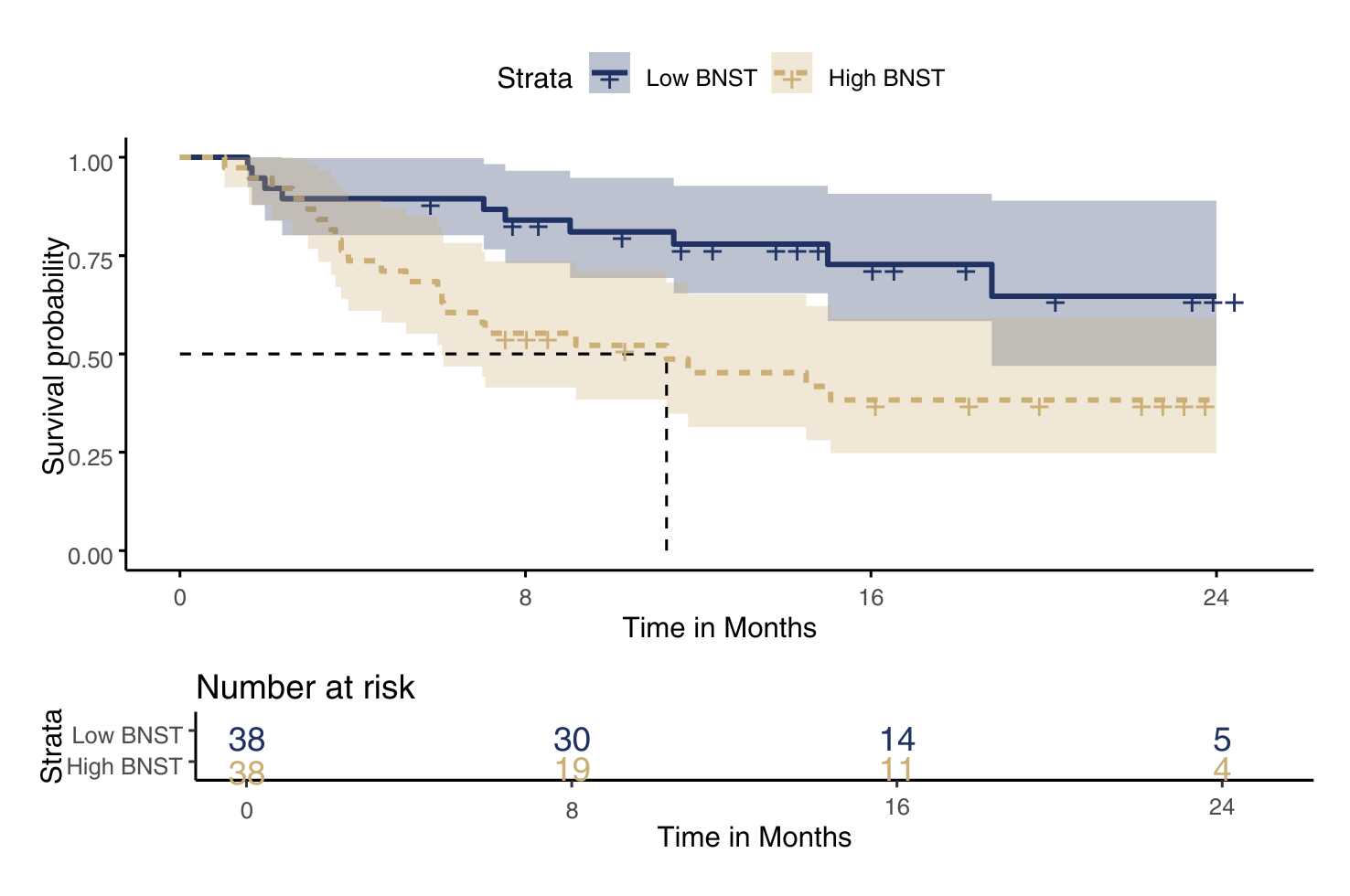
Results from the study demonstrated that older adults with remitted depression exhibited reduced stressor-evoked heart rate and systolic blood pressure reactivity, as well as reduced stressor-evoked posterior insula activation, compared with the comparison group. Within the group with remitted depression, greater stressor-evoked activity in the bed nucleus of stria terminalis was associated with a significantly faster time to relapse.
“There are several important findings and implications to this study. First, we report that older adults who have been successfully treated for their depression nonetheless show blunted brain and cardiovascular responses to stress. Importantly, however, blunted cardiovascular responses to stress in the remitted depressed group were not associated with future relapse risk. We speculate that these responses may be a homeostatic scar, reflective of past depression history and treatment, but not necessarily indicative of future risk,” said Dr. Andreescu, the study’s senior author. “Second, we identified the bed nucleus of the stria terminalis as a key node in the neural stress-related pathway that may signal an increased risk for future recurrent depressive episodes in older adults.”
Brain and cardiovascular responses to acute stress in remitted and recurrent late-life depression
Kraynak TE, Karim T, Banihashemi L, Krafty RT, Butters MA, Ajilore OA, Taylor WD, Andreescu C.
Neuropsychopharmacology. 50, 956–964 (2025). https://doi.org/10.1038/s41386-025-02057-8
